Pedal for Pat Event Raises $50,000 to Benefit the Pat Summitt Foundation
The Pedal for Pat charity cycling event announces it raised $50,000 to benefit the Pat Summitt Foundation. The 501(c)3 nonprofit, Pedal for Alzheimer’s, hosted the 12-day, 1,098-mile cycling event in honor of each of Coach Pat Summitt’s 1,098 victories. The team pedaled through five states with stops at some of the South’s finest universities to honor Summitt’s legacy and spread awareness of Alzheimer’s disease.
“The mission of the organization is made possible due to elite humans like those who pedaled, volunteered, and supported Pedal for Pat,” Josh Crisp, Board President said. “It is through generosity and commitment that we are able to support the great work of the Pat Summitt Foundation.”
The organization was pleased to team up with Lady Vol MVP and Hall of Famer Michelle Marciniak to show respect to her beloved basketball coach and mentor, the late-legendary coach Pat Summitt.
“This team accomplished so much together, and I know Pat would be proud,” Michelle Marciniak, Summitt Cyclist said. “The Pedal for Alzheimer’s organization is doing great work, and I’m proud to work with them and the Foundation to carry on the fight against Alzheimer’s in Pat’s honor.”
Marciniak continues to show dedication to making a difference in memory of Pat Summitt by reflecting on the profound impact that the legendary coach had not only on her life but on the lives of countless others.

The Pat Summitt Foundation was started by Pat and Tyler Summitt in 2011 to advance research for a cure, provide support for patients and caregivers, and promote education and awareness. The Foundation carries out its mission by supporting nonprofit organizations throughout the region, including the Pat Summitt Clinic. In conjunction with UT Medical Center, the Clinic opened its doors in 2017 and has since treated over 5,000 patients from 25 states. More information on the work of the Foundation can be found at PatSummitt.org.
“Pat was determined to beat this disease and make an impact. We are proud to continue her fight. We couldn’t have the success we do or reach the amount of patients and caregivers without the help from groups like Pedal for Alzheimer’s and the Summitt Cyclists,” said Morgan Vance, Director of Strategic Initiatives for the Pat Summitt Foundation.
The Pedal for Pat team, led by Josh Crisp and Michelle Marciniak, will present a check to the Pat Summitt Foundation at the Lady Vols basketball game at Thompson Boling Arena on Sunday, January 7th at noon EST.






























 In 2011, one month after arriving in the United States from Italy, I received the news of my grandmother’s passing. It wasn’t Alzheimer’s, but rather a brain tumor that had slowly grown over the past year. Although different, her decline in mental faculties bore striking similarities to the mental deterioration experienced by Alzheimer’s patients. Witnessing her gradual loss of the ability to perform even the simplest tasks was heart-wrenching. It was a stark reminder of the relentless nature of diseases that rob individuals of their cherished memories and abilities.
In 2011, one month after arriving in the United States from Italy, I received the news of my grandmother’s passing. It wasn’t Alzheimer’s, but rather a brain tumor that had slowly grown over the past year. Although different, her decline in mental faculties bore striking similarities to the mental deterioration experienced by Alzheimer’s patients. Witnessing her gradual loss of the ability to perform even the simplest tasks was heart-wrenching. It was a stark reminder of the relentless nature of diseases that rob individuals of their cherished memories and abilities.
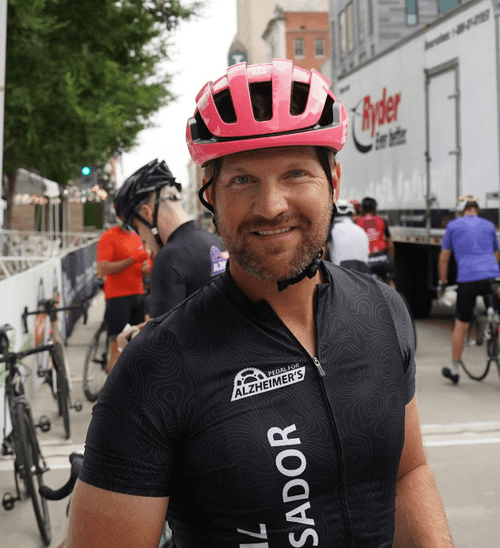
 As a veterinarian, I’ve dedicated my life to the continual improvement of my professional knowledge and competence. This commitment extends beyond the health of animals to the well-being of all living beings. Cognitive decline is a recognized condition not only in humans but also in our beloved animal companions. In the spirit of “One Health,” a collaborative approach that recognizes the interconnectedness of people, animals, plants, and the environment, I felt a calling to become an ambassador for Pedal for Alzheimer’s.
As a veterinarian, I’ve dedicated my life to the continual improvement of my professional knowledge and competence. This commitment extends beyond the health of animals to the well-being of all living beings. Cognitive decline is a recognized condition not only in humans but also in our beloved animal companions. In the spirit of “One Health,” a collaborative approach that recognizes the interconnectedness of people, animals, plants, and the environment, I felt a calling to become an ambassador for Pedal for Alzheimer’s.